Developing Ophthalmology EMR Software: A Guide for Eye Care Professionals

5 months ago
Electronic Medical Record (EMR) software is now a must-have in healthcare.
And for ophthalmologists across Canada, it’s becoming essential for keeping up with patient care demands.
EMRs can help ophthalmologists with everything from streamlining daily tasks to improving patient outcomes.
But here’s the thing: generic EMR systems often don’t fit the unique needs of eye care.
Why? Ophthalmology involves specialized exams, tests, and treatments that require precise documentation and tracking.
General EMR systems aren’t designed for this.
So, developing EMR software specifically for ophthalmology can make a big difference.
It’s all about helping eye care professionals manage their workflows, stay compliant, and provide excellent care, tailored to their field.
In this blog, we’ll dive into why customized EMR software is so crucial for Canadian ophthalmologists and explore the benefits that go beyond a one-size-fits-all solution.
Let’s take a closer look!
Why Choose Specialized Ophthalmology EMR Software?
Generic EMRs often fall short for ophthalmology. Here’s why specialized software makes a difference:
1. Tailored Templates
Specialized EMRs come with eye-specific templates and diagrams, making documentation faster and more accurate.
2. Seamless Device Integration
Direct connections to diagnostic equipment reduce manual data entry and errors, providing real-time data for better decision-making.
3. Enhanced Image Management
High-resolution image viewing tools allow for zoom, measurements, and side-by-side comparisons—critical for precise diagnosis.
Downsides of Generic EMRs
1. Reduced Efficiency: Generic systems lack ophthalmology workflows, slowing down operations and frustrating staff.
2. Limited Data Structure: Free-text entry makes reporting difficult. Specialized EMRs structure data, simplifying audits and tracking trends.
3. Missing Clinical Tools: Specialized EMRs offer decision support tools tailored for eye care, improving patient safety and outcomes.
Investing in a specialized ophthalmology EMR helps streamline your practice and deliver top-tier patient care.
Types of EMR Systems
When building EMR software, understanding the types can help you find the right fit for your practice.
1. Web-Based EMRs
These are hosted on remote servers and accessed through a web browser.
Benefits:
- Accessibility: Access from any device with internet, making remote work easier.
- Lower Startup Costs: No need for servers or IT infrastructure on-site.
Drawbacks:
- Data Ownership: The service provider owns the data, limiting your control.
- Internet Dependency: A reliable internet connection is essential, or access may be disrupted.
- Potential Slowdowns: Internet speed and traffic can impact performance.
2. Client-Server EMRs
These systems are hosted on your practice’s local servers.
Benefits:
- Speed and Performance: Local hosting means faster performance.
- Data Ownership: You own and control your data entirely.
Drawbacks:
- Higher Initial Costs: Requires investment in hardware and setup.
- Maintenance Needs: You’ll need ongoing IT support for server upkeep.
3. Hybrid EMRs
Hybrid systems combine features of both models.
Benefits:
- Data Ownership and Security: Data stays local, enhancing control and security.
- Flexible Remote Access: Secure access to local data via the internet.

Ophthalmology EMR Software Market Overview
The ophthalmology EMR market was valued at $356.1 million in 2023, with an expected growth rate of 8.7% annually through 2032.
Key factors driving this growth include:
- Rising Adoption of Digital Solutions – Practices are increasingly using EMR software to streamline patient management.
- Advanced Technologies – AI and machine learning are transforming eye care, allowing for faster, more accurate diagnostics.
- Example: AI tools can detect early signs of conditions like diabetic retinopathy and glaucoma by analyzing imaging data.
As technology advances, the demand for specialized EMR solutions in ophthalmology is only set to grow.
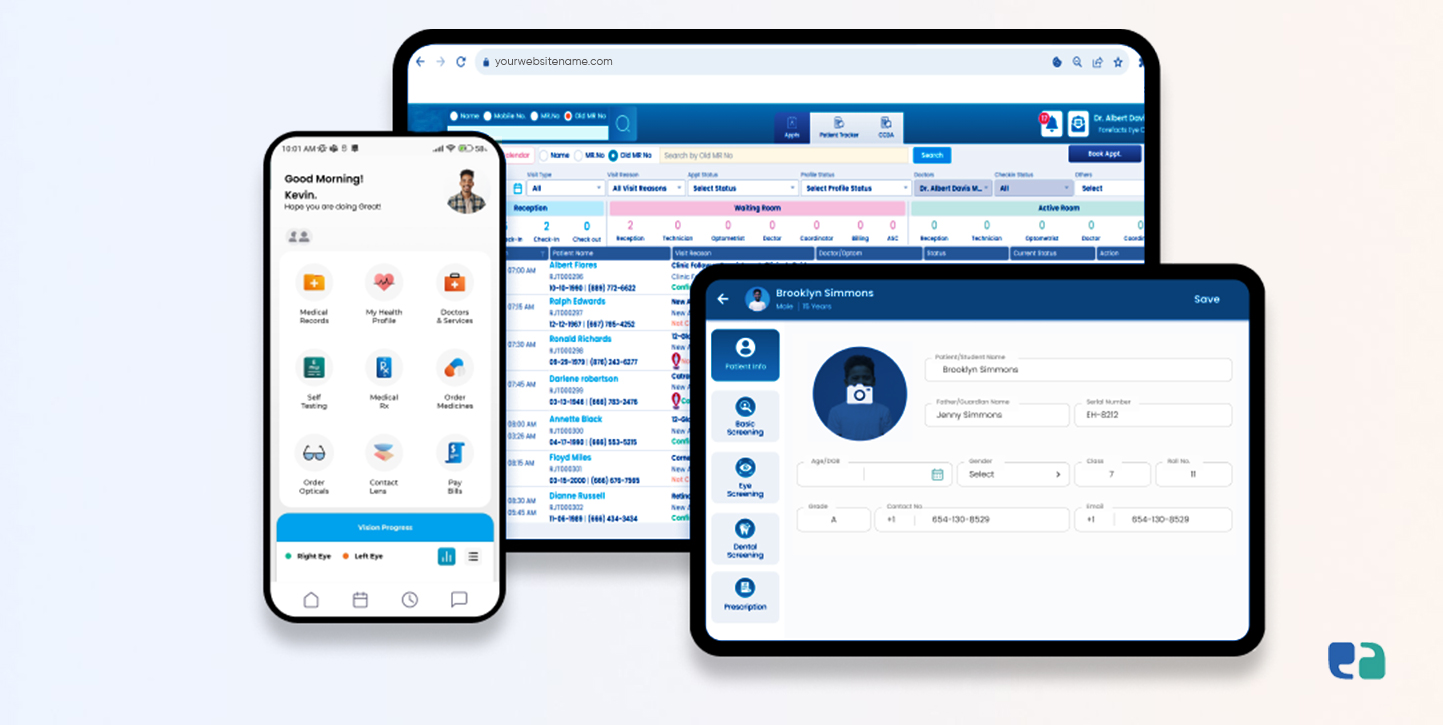
Essential Features to Add for Your Ophthalmology EMR Software
When selecting ophthalmology EMR software, look for these key features:
1. Specialty-Specific Templates
Pre-built templates for common eye conditions help streamline documentation.
Full-color anatomical illustrations aid both documentation and patient education, allowing doctors to focus more on patient interaction.
2. Diagnostic Equipment Interfaces
Integration with devices like OCT machines reduces manual data entry and errors.
This allows real-time data transfer into the EMR, improving clinical decision-making.
3. Image Viewing and Management
The EMR should efficiently handle high-resolution images, offering features like stereoscopic viewing and measurement tools to enhance diagnostic accuracy.
4. Reporting and Analytics
Robust reporting tools are essential for tracking outcomes and identifying trends.
Custom reporting can help practices monitor treatment effectiveness and improve patient care.
5. Patient Portal and Communication
A patient portal facilitates appointment scheduling, medication requests, and secure communication.
This empowers patients while ensuring compliance with HIPAA standards for privacy.
Features Specific to Ophthalmology
1. Summary Screens
Automatically display patient data over time for chronic disease management, like glaucoma. Include IOP readings and past diagnoses for a complete view.
2. Integration with Diagnostic Devices
Enable seamless data transfer from modern diagnostic tools directly into the EMR, eliminating manual entry and inefficiencies.
3. Image Viewing and Interpretation
Offer high-quality image viewing with features like stereoscopic analysis and measurement tools to enhance diagnostic accuracy.
4. Subspecialty Modules
Create tailored EMR versions for different subspecialties, such as glaucoma and retina, with specific templates and workflows.
5. Lens Calculations
Provide detailed IOL power calculations for cataract surgery, improving lens selection and surgical outcomes.
These features enhance the functionality of EMR software, making it essential for ophthalmology practices.
The Software Development Journey for Ophthalmology EMR
1. Planning and Requirements Gathering
Ophthalmologists need to identify their specific needs by understanding the challenges in their practice and defining software requirements.
For instance, a glaucoma-focused practice may require features for tracking visual field changes and IOP measurements. Involving clinicians early helps ensure the software meets practical needs and improves patient care.
2. Selecting a Development Team
Ophthalmologists can choose between two main options:
- In-House Development Team: This gives more control and customization but requires significant investment in recruiting and training.
- Outsourcing: Working with a specialized healthcare software company brings expertise in regulations and best practices. Look for a partner with a strong track record in ophthalmology EMR development.

3. Design and Development
It involves creating prototypes, testing with users, gathering feedback, and refining the software. This flexibility ensures the final product fits user needs.
4. Testing and Quality Assurance
Testing is crucial to ensure the software works well, is secure, and integrates smoothly with diagnostic devices. Security is especially important to protect sensitive patient information and comply with PIPEDA/HIPAA.
5. Deployment and Implementation
Deployment involves installing the software and integrating it with existing systems. Key steps include:
- Data Migration: Moving patient data from old systems to the new one.
- Staff Training: Training all users on how to use the EMR effectively.
- Ongoing Support: Providing help and maintenance to address technical issues.
Importance of Security and Compliance in Ophthalmology EMR
Data security is essential in ophthalmology EMR software.
Protecting patient information prevents breaches, especially since healthcare is a target for cyberattacks.
The 2021 Eye Care Leaders EMR breach affected over 1.5 million individuals, highlighting the need for strong security measures like access controls and data encryption.
In Canada, compliance with the Personal Information Protection and Electronic Documents Act (PIPEDA) is crucial.
This includes implementing security measures, conducting risk assessments, and training staff on handling personal health information (PHI).
Failing to comply can lead to serious penalties and damage to a provider's reputation.
By prioritizing security and compliance, providers can protect patient privacy and build trust with their users.
Benefits Beyond Clinical Care in Ophthalmology EMR
Implementing an EMR in an ophthalmology practice comes with many advantages beyond just clinical care.
1. Financial Benefits
- Improved Coding Accuracy: EMRs help with accurate coding during exams, which can boost revenue by reducing undercoding.
- Reduced Administrative Staff: Moving to electronic charts streamlines workflows and may lower the need for administrative support.
- Streamlined Billing: EMRs simplify billing with features like electronic superbills and automated charge capture, making the process much more efficient.
2. Enhanced Communication
- Electronic Referrals: Secure electronic transmission of referrals speeds up the process and improves coordination.
- Messaging within EMR: Built-in messaging allows team members to communicate quickly, enhancing collaboration.
- Customized Letters: Generate tailored letters for referring doctors and patients, improving overall communication.
3. Error Prevention
- Automated Data Entry: Integrating diagnostic devices with EMRs cuts down on manual data entry errors.
- Electronic Prescriptions: E-prescribing reduces mistakes from handwritten notes, ensuring safer medication management.
4. Clinical Governance and Research
- Clinical Audits: EMRs make it easier to conduct audits and monitor quality standards.
- Research Data Collection: Structured data helps identify patients for research and streamlines data collection.
- Tracking Clinical Outcomes: EMRs allow practices to track patient outcomes over time, supporting quality improvement efforts.